Say No To Heart Disease: The drug-free guide to preventing and fighting heart disease
The good news is that there are steps to take to reduce your risk for heart disease if you have diabetes.
The best way to prevent heart disease is to take good care of yourself and your diabetes.
1.Control Your Weight
One of the most important things you can do if you have diabetes is maintain a healthy weight. If you are overweight, talk to a registered dietitian about healthy ways to lose weight.
If you are overweight, you are more likely to develop cardiovascular diseases, diabetes, or certain cancers.
The increased health risk of obesity is most marked when the excess fat is mainly in the tummy (abdomen) rather than on the hips and thighs.
As a rule, a waist measurement of 102 cm or above for men (92 cm for Asian men) and 88 cm or above for women (78 cm for Asian women) is a significant health risk.
2.Get Regular Physical Activity
There is a significant body of research that proves the numerous cardiovascular benefits of regular physical activity (that goes beyond weight loss). Start off slowly, and build a plan that works well for you and meets your needs.
People who are physically active have a lower risk of developing cardiovascular diseases compared with inactive people. To gain health benefits you should do at least 30 minutes of moderate physical activity, on most days (at least five days per week).
30 minutes in a day is probably the minimum to gain health benefits. However, you do not have to do this all at once. For example, cycling to work and back 15 minutes each way adds up to the total of 30 minutes.
Moderate physical activity means that you get warm, mildly out of breath, and mildly sweaty. For example, brisk walking, jogging, swimming, cycling, etc. However, research studies do suggest that the more vigorous the exercise, the better for health – particularly for preventing heart disease.
On most days. You cannot store up the benefits of physical activity. You need to do it regularly.
3.Maintain Tight Control Over Glucose
Tight control can prevent many complications from diabetes and also protects your heart. Aim for an A1C reading of less than 7%.
The increased risk that diabetes and kidney disease pose to developing cardiovascular diseases can be modified. For example, good control of blood sugar (glucose) levels in people with diabetes reduces the risk. Good control of blood pressure in people with diabetes and kidney diseases reduces the risk.
4.Lower Your LDL Cholesterol (the “bad” type)
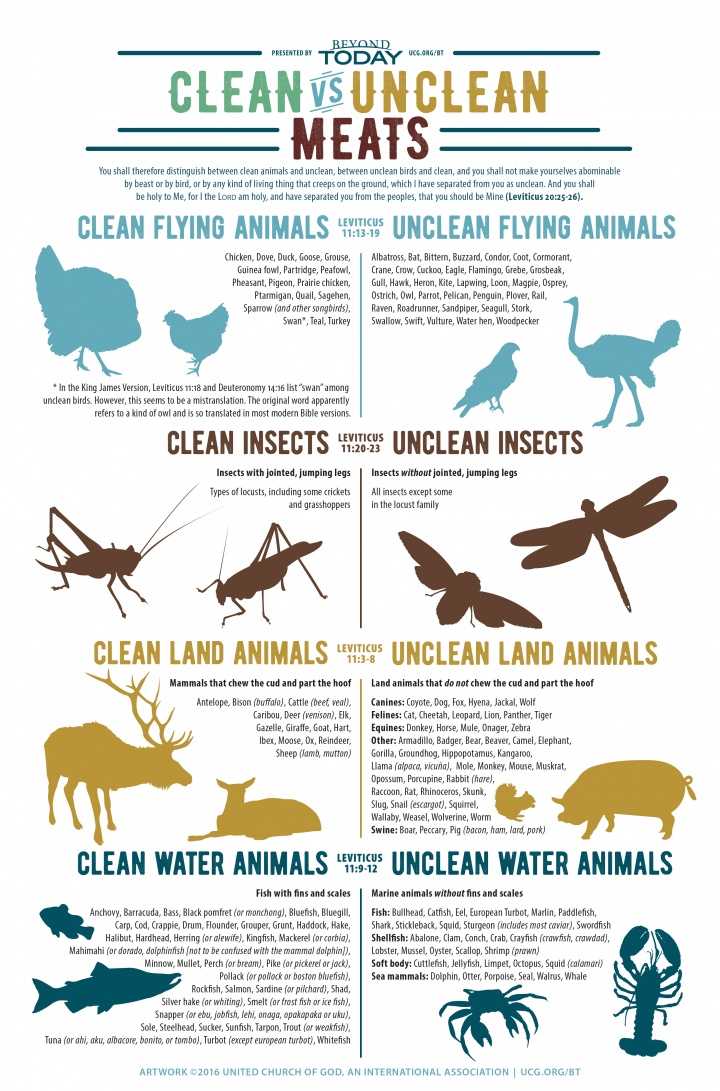
An LDL cholesterol goal of less than 100 mg/dl is recommended. Eat fiber-rich foods, such as fruits, vegetables, and whole grains. Also, omega-3 fish oil supplements is recommended.
Eating healthily helps to control obesity, and lower your cholesterol level. Both of these help to reduce your health risk.
Also, there is some evidence that eating oily fish (herring, sardines, mackerel, salmon, kippers, pilchards, fresh tuna, etc) helps to protect against heart disease.
Also, fruit and vegetables, as well as being low in fat, also contain antioxidants and vitamins .
Briefly, a healthy diet means:
AT LEAST five portions, or ideally 7-9 portions, of a variety of fruit and vegetables per day.
A THIRD OF MOST MEALS should be starch-based foods (such as cereals, wholegrain bread, potatoes, rice, pasta), plus fruit and vegetables.
NOT MUCH fatty food such as fatty meats, cheeses, full-cream milk, fried food, butter, etc. Use low-fat, mono-unsaturated or polyunsaturated spreads. One study conducted at Harvard University found that replacing saturated fats with polyunsaturated fats is an effective way of lowering your risk of heart attacks and other serious problems from heart disease.
INCLUDE 5 portions of fish per week, at least three of which should be oily (such as herring, mackerel, sardines, kippers, salmon, or fresh tuna).
LIMIT SALT to no more than 5 g a day (and less for children). This is about a teaspoon of salt. Even a modest reduction in intake can make quite a big difference.
About three quarters of the salt we eat is already in the foods we buy. Simply checking food labels and choosing foods with lower salt options can make a big difference.
Avoid all types of processed foods especially those with a high salt content such as packaged foods and high salt meats such as bacon and rashers.
These are especially bad for your health!
Also dont add salt to food at the table!
If you eat meat, it is best to eat lean meat, or poultry such as chicken.
If you do fry, choose a vegetable oil such as sunflower, rapeseed or olive.
5.Control Your Blood Pressure
All people with diabetes should aim for a blood pressure reading of less than 130/80.
You should have your blood pressure checked at least every year. High blood pressure usually causes no symptoms, so you will not know if it is high unless you have it checked. However, over the years, high blood pressure may do some damage to the blood vessels (arteries) and put a strain on your heart.
High blood pressure can be lowered by losing weight if you are overweight, regular physical activity and eating healthily as described above. Medication may be advised if your blood pressure remains high.
6.Consider Incorporating Aspirin Into Your Daily Routine
If you are older than thirty years of age, you may want to speak to your doctor about taking a baby aspirin daily. In addition, taking a multivitamin can be extremely helpful for those of us with diabetes.
7.Benefits of Quitting Smoking and Avoiding Secondhand Smoke
One of the best ways to reduce your risk of heart disease is to avoid tobacco smoke. Don’t ever start smoking. If you already smoke, quit.
No matter how much or how long you’ve smoked, quitting will benefit you.
Also, try to avoid secondhand smoke. Don’t go to places where smoking is allowed. Ask friends and family members who smoke not to do it in the house and car.
Quitting smoking will reduce your risk of developing and dying from heart disease. Over time, quitting also will lower your risk of atherosclerosis and blood clots.
If you smoke and already have heart disease, quitting smoking will reduce your risk of sudden cardiac death, a second heart attack, and death from other chronic diseases.
Researchers have studied communities that have banned smoking at worksites and in public places. The number of heart attacks in these communities dropped quite a bit. Researchers know these results are due to a decrease in active smoking and reduced exposure to secondhand smoke.
8.Calculating Your Cardiovascular Health Risk
A ‘risk factor calculator’ is commonly used by GPs and practice nurses. This can assess your cardiovascular health risk. A score is calculated which takes into account all your risk factors such as age, sex, smoking status, blood pressure, cholesterol level, etc.
The calculator has been devised after a lot of research that monitored thousands of people over a number of years. The score gives a fairly accurate indication of your risk of developing a cardiovascular disease over the next 10 years.
Who should have their cardiovascular health risk assessed?
Current guidelines advise that the following people should be assessed to find their cardiovascular health risk:
All adults aged 40 or more.
Adults of any age who have:
A strong family history of early cardiovascular disease. This means if you have a father or brother who developed heart disease or a stroke before they were aged 55; or, if you have a mother or sister who developed heart disease or a stroke before they were aged 65.
A first-degree relative (parent, brother, sister, child) with a serious hereditary lipid disorder.
If you already have a cardiovascular disease or diabetes then your risk does not need to be assessed. This is because you are already known to be in the high-risk group.
I am a great lover of style!Especially nice clothes!
I was in the Swords Shopping Centre yesterday where I picked up a lovely outfit for my birthday!
I think that retail therapy is great for the heart what do you think?
Retail therapy is a great incentive to go walking which is great for the heart!It makes you feel good when you buy things for yourself and other people!
People think that spending money isnt the best thing to do for your heart but it is!By spending money on other people your heart is happy!
It makes you focus on buying nice things rather than worrying about things!So that reduces stress!
I think that people feel better about themselves when they are all dressed up what do you think?
I took a photo of the new outfit I bought for my birthday you can see it in the picture below!
I got the top and trousers in Dunnes Stores and the nude shoes in Clarks!

What does the assessment involve?
A doctor or nurse will:
Do a blood test to check your cholesterol and blood sugar (glucose) level.
Measure your blood pressure and your weight.
Ask you if you smoke.
Ask if there is a history of cardiovascular diseases in your family (your blood relations); if so, at what age the diseases started in the affected family members.
A score is calculated based on these factors plus your age and your sex. An adjustment to the score is made for certain other factors such as strong family history and ethnic origin.
What does the assessment score mean?
You are given a score as a percentage chance. So, for example, if your score is 30%, this means that you have a 30% chance of developing a cardiovascular disease within the next 10 years. This is the same as saying a 30 in 100 chance (or a 3 in 10 chance).
In other words, in this example, 3 in 10 people with the same score that you have will develop a cardiovascular disease within the next 10 years.
Note: the score cannot say if you will be one of the three. It cannot predict what will happen to each individual person. It just gives you the odds.
You are said to have a:
High risk – if your score is 30% or more. This is a 3 in 10 chance or more of developing a cardiovascular disease within the next 10 years.
Moderate risk – if your score is 10%. This is a 1 in 10 chance or more of developing a cardiovascular disease within the next 10 years. This should be re-assessed every year.
Low risk – if your score is less than 10%. This is less than a 1 in 10 chance or more of developing a cardiovascular disease within the next 10 years.. This should be re-assessed every year.
9.How Stress Causes Cardiovascular Disease

Treating the Aching Heart: A Guide to Depression, Stress and Heart Disease
Living a stressful life can cause people to adopt poor habits like smoking and eating badly, which in turn are risk factors for cardiovascular disease.
But being stressed itself can alter the way the body behaves and this can bring about changes to the blood and nervous system, which can have negative effects on your heart health.
Studies show that acute stress triggers reduced blood flow to the heart, promotes your heart to beat irregularly and increases the likelihood of your blood clotting. All of these can trigger the development of cardiovascular disease.
If you already have atherosclerosis and become acutely stressed you may experience chest pains caused by the arteries to your heart contracting and reducing the blood flow.
When experienced over an extended period of time, all these effects can cause damage to the lining of the blood vessels. This makes the blood vessels more susceptible to atherosclerosis.
For more great Health and Nutrition Tips refer to the website positivehealthwellness.com.
If you have any information,questions, or feedback you would like to include in this post.
Please email momo19@diabetessupportsite.com or leave your comments below.