Just like high blood glucose makes it easier for you to get an infection in other places in your body, high blood glucose levels also make it easier to get a gum infection, or other infection in your mouth.
The high blood sugar level makes it easier for bacteria to thrive and multiply. Plaque is a colorless, sticky collection of bacteria; if it hardens into tartar and isn’t removed in time, then cavities form.
One of the warning signs of diabetes is increased thirst. Diabetes inhibits the salivary glands, making the mouth feel dry. Saliva is needed to wash away plaque, so if you have less saliva, you could have more plaque which leads to tooth decay.
An infection in your gums may be a reason why you are unable to keep your blood glucose in a good range. An infection anywhere in your body could be a reason for unruly blood glucose.
Decaying teeth and poor oral habits contribute to periodontal disease, as does smoking. Periodontal disease is an infection that develops of the gum, and underlying bone, that holds the teeth in place.
When periodontal disease is left unchecked, it can lead to worsening blood glucose control, due to the fact that there is bacteria in the gum or bone that hold the teeth in place. Chewing can also become painful, and loss of teeth may occur.
What Is Periodontal Disease?
Cure Gum Disease Naturally: Heal Gingivitis and Periodontal Disease with Whole Foods
The most common and well known form of gum disease is gingivitis. The condition involves the inflammation of the gingiva or gums surrounding the necks of the teeth, and is caused by plaque developing along the gumline.
Symptoms include red and swollen gums, as well as gum bleeding, which can be seen on your toothbrush or at a dental exam. Often noticeable through bad breath, gingivitis can also be caused by a number of health conditions or medical changes in an individual.
Fortunately, there is no bone loss around the teeth from the development of gingivitis, and it can be easily treated or prevented. A quality soft toothbrush, especially a battery-powered one, should be used twice a day to decrease the risk of developing gingivitis.
Flossing will further reduce the chances of developing the disease, as will other common oral hygienic practices: mouth rinses, water picks and interproximal cleansing devices.
The second-most common periodontal disease is “periodontitis.” Like gingivitis, it is caused by bacterial plaque, but it can cause loss of bone support within the teeth. It can be treated or prevented, but rarely can the damage be reversed. Periodontitis can occur if gingivitis is left untreated.
Signs of periodontitis, like gingivitis, include red and swollen gums, and bleeding. The formation of gum pockets around the teeth may also occur, which is defined by an opening around the gum tissue of the teeth. This allows bacteria and the formation of tartar to get deeper under the gum line. This deepening of the pocket is associated with bone loss, and can lead to tooth loss if left untreated.
Uncontrolled diabetes, obesity, genetic susceptibility and poor oral hygiene can all heighten a person’s risk of developing periodontitis. Untreated periodontits can not only yield tooth loss, but create systemic health issues such as an increased risk of cardiovascular (heart) disease.
How Periodontal Disease Affects Diabetes
People with diabetes are more likely to have periodontal disease than people without diabetes, probably because people with diabetes are more susceptible to contracting infections. In fact, periodontal disease is often considered a complication of diabetes. Those people who don’t have their diabetes under control are especially at risk.
Other lifestyle factors such as obesity, physical activity and diet are also likely to affect the risk of periodontitis.
Research has suggested that the relationship between diabetes and periodontal disease goes both ways – periodontal disease may make it more difficult for people who have diabetes to control their blood sugar.
Severe periodontal disease can increase blood sugar, contributing to increased periods of time when the body functions with a high blood sugar. This puts people with diabetes at increased risk for diabetic complications.
Good blood glucose control is key to controlling and preventing mouth problems. People with poor blood glucose control get gum disease more often and more severely than people whose diabetes is well controlled.
Other problems diabetes can cause are dry mouth and a fungal infection called thrush. Dry mouth happens when you do not have enough saliva—the fluid that keeps your mouth wet. Diabetes may also cause the glucose level in your saliva to increase. Together, these problems may lead to thrush, which causes painful white patches in your mouth.
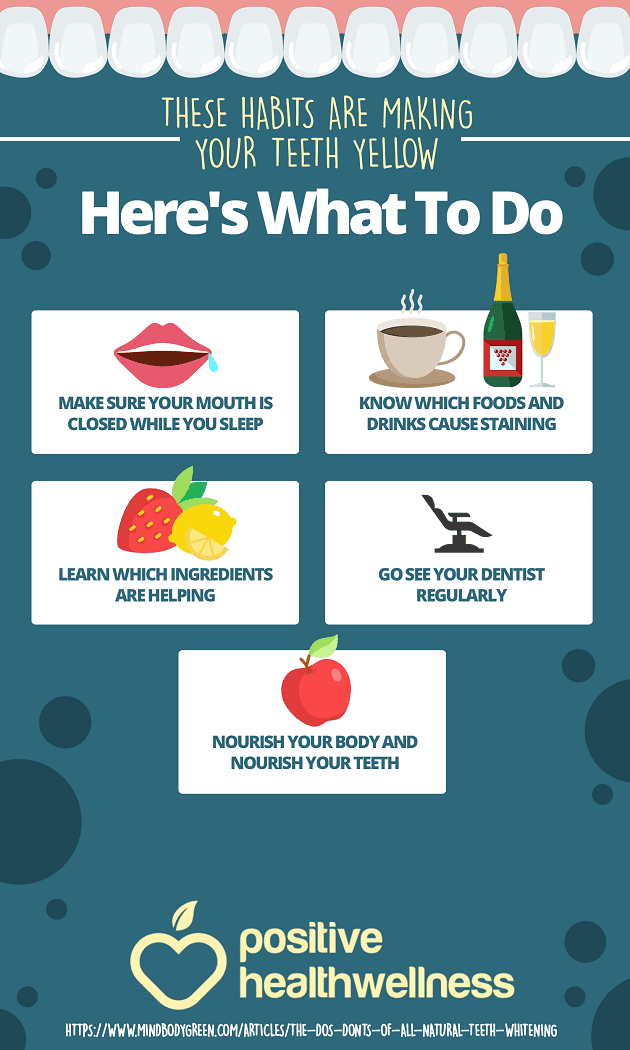
Daily brushing and flossing, regular dental check-ups and good blood glucose control are the best defense against the oral complications of diabetes.
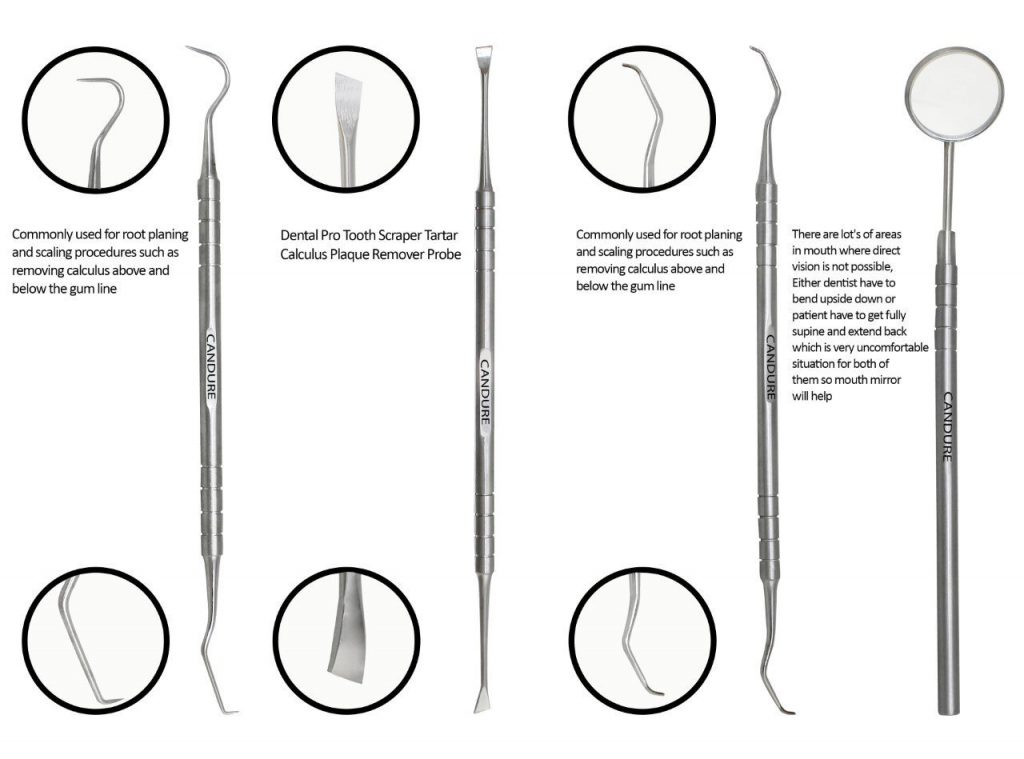
A sensitive toothbrush is always the first step, and proper oral hygiene is a must to help prevent peridontitis. If you’re a smoker, quitting is also highly recommended. Treatment of peridontitis by your dentist and hygienist will include deep cleanings, called scaling and root planing, but more serious areas of bone loss around the teeth may require gum surgery, including gum and bone grafts.
Keep in mind: After the periodontits is controlled, it is never truly cured. Seek frequent annual cleanings to prevent long-term problems.
Other common Dental Problems from Diabetes
Infection and delayed healing – Diabetes lowers your resistance to infection, delays healing and can complicate gum and oral surgeries. It may also be difficult to control your blood sugar levels after surgery. Doctors ask for blood glucose levels to be checked before any invasive oral procedure or surgery. In case the diabetes is not well controlled, the procedure is usually deferred.
Increased tooth decay – Bacteria in the mouth interact with starches and sugars in food to form plaque on your teeth. In diabetics, the increased blood sugar level increases your risk of tooth decay.
Thrush
Thrush is a fungus of the oral cavity, or mouth. With diabetes, high glucose causes fungus levels to rise in the mouth. Wearing dentures, or smoking, also increases the risk of thrush. An oral suspension is usually given to the patient to swish and swallow several times per day to cure this infection. To prevent it, keep your diabetes in check, clean dentures regularly, and do not smoke or use tobacco products.
Dry mouth
Dry mouth can cause your mouth to be sore, can cause infections or ulcers in the mouth, or even tooth decay. It is sometimes a sign that a person has diabetes. This is because when your mouth is dry, there is no saliva. Saliva provides protection against bacteria. Saliva coats teeth with needed minerals, and washes away food particles from around teeth. This promotes the growth of microorganisms in the mouth that can cause gum infection or tooth decay.
Be sure to check with your pharmacist that your medications are not causing your mouth to dry. Many over the counter and prescription medications can cause dry mouth, in fact the list is quite extensive.
Artificial saliva may be prescribed, and may help with the symptom of dry mouth, while not only uncomfortable, can contribute to periodontal disease. Again, good control of blood glucose is key to preventing dry mouth.
Oral burning
If blood glucose levels are not controlled well, it can lead to a condition known as oral burning. A bitter taste may accompany the burning sensation, along with dry mouth. Often these symptoms get worse as the day goes on.
Other common symptoms include:
A mouth ulcer or sore in the mouth that won’t heal
Holes in your teeth or dark spots
Mouth, jaw, or face pain
Loose teeth
Problems with chewing, including pain
A bad taste in the mouth, or change in sense of taste, or bad breath that doesn’t go away with brushing
Dental Tips for Diabetics
The following are some tips that people with diabetes should follow in order to prevent dental problems.
1.Keep your blood glucose in your target range, with an A1C of less than 7 percent (or as specified by your doctor)
2.See your dentist for regular six month check-ups and cleanings, or even more often if your dentist recommends it or when you develop a problem with your teeth or gums in between visits
3.Tell your dentist that you have diabetes, and let him or her know your recent diabetes numbers (A1C, recent blood glucose reading)
4.Brush teeth at using gentle circular motions at least twice daily with a soft bristle tooth brush using fluoride toothpaste, and don’t forget to brush your tongue and get a new toothbrush every three months
5.Floss daily using a long piece of dental floss, working your floss along the gum line and up each tooth, and rinse well following flossing (if your gums bleed, keep flossing! They will toughen up in time)
6.Use an anti-plaque mouth rinse to help prevent plaque build up
7.Use a dental pick or brush, which are tools that can get between the teeth better than a toothbrush
8.Keep dentures clean, and remove them at night and get adjusted if they don’t fit right
9.Gummy or hard candies, sodas, processed fruit snacks or dried fruits, all of these are full of sugar that adheres to the teeth and feeds oral bacteria.
So don’t let that plaque and the oral bacteria with it damage your teeth. Limit your sugar consumption to reasonable amounts, and brush regularly.
10.Including more calcium in your diet isn’t just about building strong bones, it’s also great for your teeth.
11.Fruits and vegetables contain significant quantities of vitamin C and vitamin A, which are important for healthy gums and building enamel.
Here are some good options:
Apples,Bananas,Pineapples,Cucumbers,Strawberries,Carrots,Watermelon,Celery and Garlic.
Try and include as many vegetables and fruit in your diet as you can, assuming they are not just good for your teeth, but for your whole body as well.
12.While you should quit smoking for a numerous other reasons, quitting will also be better for your teeth and gums.
Smoking weakens your immune system, making it harder for your mouth to fight off a gum infection. As a matter of fact, smokers have twice the risk for gum disease compared with a nonsmoker.
And, after the infection damages the gums, continuing smoking makes it more difficult for your gums to heal.
And it’s not just smoking. Consuming tobacco in all its forms – cigarettes, spit tobacco, pipes – can raise your risk for gum disease. So please, quit using tobacco.
13.Mucosal cells in our mouths turn over within three to seven days. So nutrient shortfalls or excesses will show up in mouth tissue before they show up anywhere else.
Periodontal disease is associated with lower blood levels of vitamins and minerals. And getting enough of specific nutrients can be important to successful treatment.
| Nutrient | What you need it for |
|---|---|
| Protein | Tooth structure, mucosal/connective tissue development, and immune function. |
| Calcium | Tooth structure; may enhance enamel remineralization. |
| Phosphorus | Tooth structure. |
| Zinc | Mucosal/connective tissues and immune function. |
| Antioxidants | Mucosal/connective tissues and immune function. |
| Folate | Mucosal/connective tissues and immune function; low levels are associated with periodontal disease. |
| Iron | Mucosal/connective tissues and immune function. |
| Vitamin A | Mucosal/connective tissues and immune function. But be aware that getting too much from supplements may result in gum problems. |
| Vitamin C | Collagen maturation and to maintain the integrity of the periodontal ligament; mucosal/connective tissues and immune function. |
| Omega-3 fats | Mucosal/connective tissues and immune function; modulates the inflammatory response. |
| Vitamin D | Mucosal/connective tissues, immune function; may enhance enamel remineralization. |
| B vitamins | Epithelial cell turnover. |
Try to get the nutrients mentioned above from whole foods. (Bonus: You give your teeth and gums a workout!) Unless you have a known deficiency, supplements should not be necessary.
14.It is our responsibility to make sure that we take good care of our teeth and gums. Moreover, this does not only mean going to the dentist and brushing our teeth regularly. This also means practicing proper oral care and hygiene.
Click the following link for How To Get Rid Of Gum Disease
If you have any information,questions, or feedback you would like to include in this post.
Please email momo19@diabetessupportsite.com or leave your comments below.